

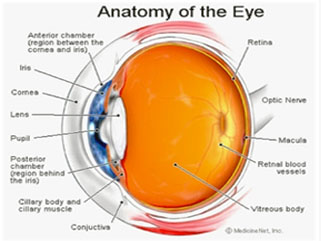
AMD ( age related macular degeneration) is a condition that occurs when cells in the macula degenerate. Damage to the macula affects your central vision which is needed for reading, writing, driving, recognizing people's faces and doing other fine tasks. This loss of central vision will severely affect normal sight.
AMD can affect anyone. It becomes more common with increasing age. If you develop AMD in one eye, you have a high chance (about 6 in 10) that it will also develop in the other eye.
About 5 in 100 people aged over 65 have AMD severe enough to cause serious visual loss.
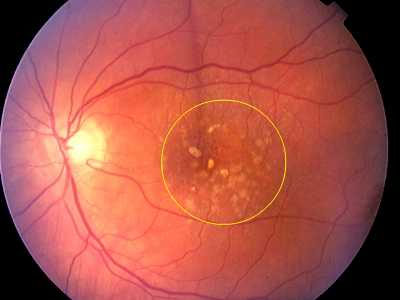
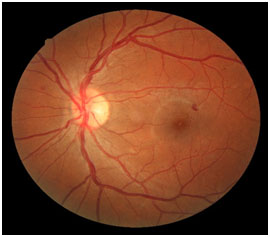
This is the most common form. In this type the cells in the RPE of the macula gradually become thin, degenerate and dry. This layer of cells is crucial for the function of the rods and cones which then also degenerate and die. Typically, dry AMD is a very gradual process and usually takes several years for vision to become seriously affected.
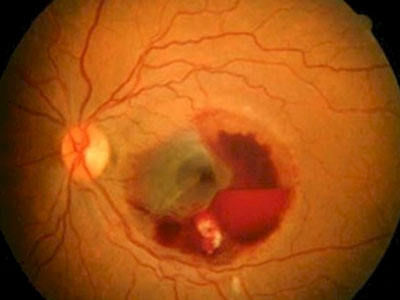
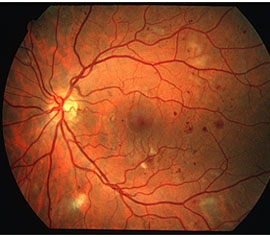
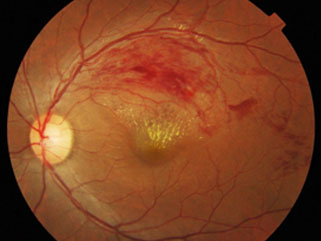
Wet AMD may also be called neovascular or exudative AMD. It occurs in about 1 in 10 cases. However, it is likely to cause severe and sudden visual loss over quite a short time - sometimes just months. In wet AMD, in addition to the retinal pigment cells degenerating, new tiny blood vessels grow from the tiny blood vessels in the choroid. This is called choroidal neovascularisation. These vessels are not normal. They are fragile and tend to leak blood and fluid. This can damage the rods and cones, and cause scarring in the macula, causing further vision loss.
In people with AMD the cells of the RPE do not work so well with advancing age. They gradually fail to take enough nutrients to the rods and cones, and do not clear waste materials and byproducts made by the rods and cones either. As a result, tiny abnormal deposits called drusen develop under the retina. In time, the retinal pigment cells and their nearby rods and cones degenerate, stop working and die. Sometimes it also triggers new blood vessels to develop from the choroid.
Certain risk factors increase the risk of developing AMD. These include:

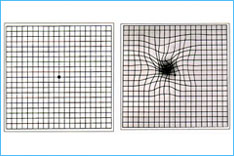
Always see a retina doctor promptly if you develop visual loss or visual distortion.
The ophthalmologist will examine the back of your eye with a slit lamp microscope to evaluate your retina.
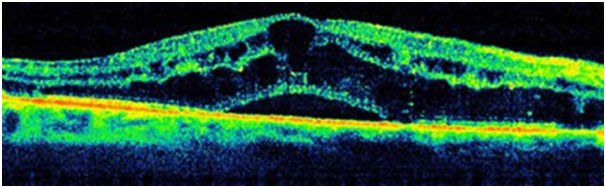
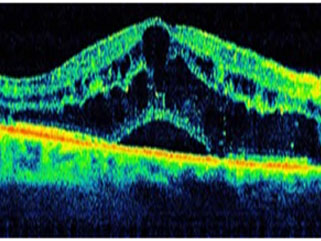
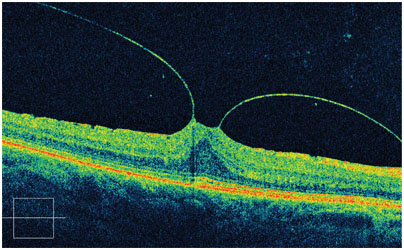
OCT is done to get very detailed '3D' information about the macula. It is also a useful test to assess and monitor the results of any treatment.
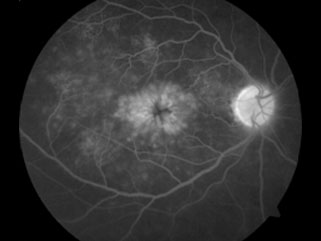
FFA (fluorescein angiography) is done in which a dye is injected into a vein in your arm. Then, by taking pictures with a special camera, the ophthalmologist can see where any dye leaks into the macula from the abnormal leaky blood vessels. This test can give an indication of the extent and severity of the condition.
For the more common dry AMD, there is no specific treatment yet. There are, however, certain things that can be done to maximize the sight you do have and to improve your eye health. Low vision rehabilitation and low vision services are offered by hospital eye departments and information can be found from the National Institute of Blind People (RNIB). Stopping smoking and protecting the eyes from the sun's rays by wearing sunglasses are important. A healthy balanced diet rich in antioxidants may be beneficial, as may the addition of dietary supplements (see below for details). Remember that in this type of AMD the visual loss tends to be gradual, over 5-10 years or so.
For the less common wet AMD, treatment may halt or delay the progression of visual loss in some people. Newer treatments may even be able to reverse some of the visual loss. Treatments which may be considered include treatment with anti-vascular endothelial growth factor (anti-VEGF) medicines, photodynamic therapy and laser photocoagulation.
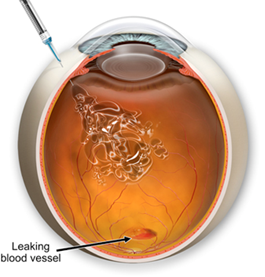
In recent years a group of medicines called anti-VEGFs has been developed. Vascular endothelial growth factor is a chemical that is involved in the formation of new blood vessels in the macula in people with wet AMD. By blocking the action of this chemical, it helps to prevent the formation of the abnormal blood vessels that occur in wet AMD. Avastin and Lucentis are two such injections.
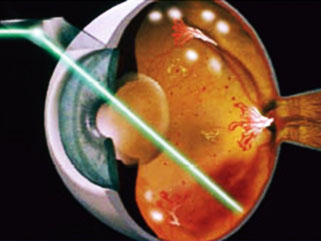
The anti-VEGF medicines are injected using a fine needle directly into the vitreous of the eye. Repeat Anti VEGF injections are needed every four weeks. A loading dose of 3 injections given a months interval is used followed by additional injections if required. On average a patient would require about 5-6 injections per year
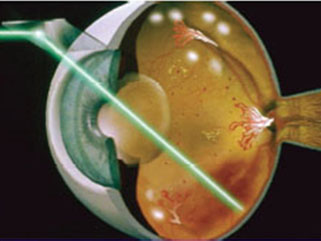
Photodynamic therapy
A medicine called verteporfin is injected into a vein in the arm. Within a few minutes the verteporfin binds to proteins in the newly formed abnormal blood vessels in the macula. A light at a special wavelength is then shone into the eye for just over a minute which activates verteporfin and causes damage, destroying the abnormally growing blood vessels (neither damaging the nearby rods and cones, nor any normal blood vessels). Success means that the visual loss is prevented from getting worse - it does not restore any lost vision. Treatment usually needs to be repeated every few months to continue to suppress newly growing blood vessels. The main advantage that this method has is less damage to the normal retina.
Certain groups of people with AMD (both wet and dry types) can benefit from vitamin and mineral supplements. These supplements can slow down the progression of AMD.
A specific combination of high-dose vitamins and minerals has been tested and found to be most effective. The mixture includes vitamin C 500 mg, vitamin E 400 IU, lutein 10 mg, zeaxanthin 2 mg, zinc oxide minimum 25 mg and cupric oxide daily.
There is some concern that Beta-carotene has been found to increase the risk of lung cancer in smokers, so these supplements are not advised in either ex-smokers or current smokers. Zinc may increase the risk of developing bladder and kidney problems.
When your vision becomes poor, it is common to be referred (by your ophthalmologist) to a low vision clinic. Staff at the clinic provide practical help and advice on how to cope with poor and/or deteriorating vision.
Help may include:
ALWAYS REMEMBER TO GET YOUR RETINA CHECKED TWICE A YEAR.
Diabetic retinopathy (DR) is the most common type of diabetic eye disease and the leading cause of blindness. Diabetes causes damage to the blood vessels of the retina, a thin and delicate tissue that is responsible for vision. In some people suffering from DR, blood vessels swell and leak fluid. In others, abnormal new blood vessels grow on the surface of the retina that can lead to bleeding and retinal detachment. A healthy retina is necessary for good vision.
If you have diabetic retinopathy, at first you may not notice changes to your vision. Yet over time, the condition can worsen and cause vision loss. Diabetic retinopathy usually affects both eyes, but early detection and prompt treatment can minimize vision loss.
Moderate Nonproliferative Retinopathy
Moderate nonproliferative retinopathy is essentially a progression from the mild stage. Many more microaneurysms, hemorrhages and cotton wool spots emerge and there is further damage to the retinal blood vessels. The danger is that such damage can result in reduced blood flow to the surrounding retinal tissue leading to vision loss.
Mild Nonproliferative Retinopathy
The features of mild nonproliferative retinopathy are some of the earlier stages of diabetic retinopathy. At this point, small areas of balloon-like dilation of blood vessels, called microaneurysms, start to appear along with other findings such as small spot hemorrhages and cotton wool spots. It's important to note that not all patients with mild nonproliferative retinopathy will notice a change in their vision.
Severe Nonproliferative Retinopathy
As the retinopathy progresses and more blood vessels have now been affected, larger areas of the retina are deprived of blood flow, these are known as capillary non perfusion areas. This results in the retina producing new blood vessels in an attempt to enhance nourishment.
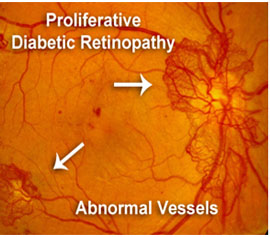
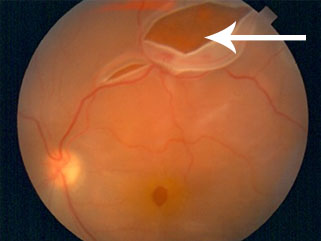
Proliferative Retinopathy
At this advanced stage, the signals sent by the retina for nourishment trigger the growth of new blood vessels that grow along the retina and into other parts of the eye. These blood vessels are abnormal and fragile, often leading to the development of new or worsening existing symptoms and frequent vision loss. Left untreated, severe vision loss and even permanent blindness can result.

Damaged blood vessels from diabetic retinopathy can cause vision loss in several ways:
All diabetics—both Types 1 & 2—are at risk, which is why everyone with diabetes should get a comprehensive dilated eye exam at least once a year. The longer someone has diabetes, the more likely he or she will develop diabetic retinopathy. It's fortunate that in most cases diabetic retinopathy is a treatable condition.
Diabetic retinopathy may be a problem for women with diabetes during pregnancy. To protect vision, every pregnant woman with diabetes should have a comprehensive dilated eye exam as early as possible.
DIALATED EYE EXAMS
Early detection and treatment can prevent vision loss. If you are diabetic, be sure to schedule a comprehensive dilated eye exam at least twice a year. It is important to remember that your diabetic retinopathy can progress without symptoms. You can develop both proliferative retinopathy and macular edema and still see normally, but you may remain at high risk for vision loss. A retina specialist can tell if you have any stage of diabetic retinopathy or macular edema. Depending on the severity of your diabetic retinopathy, your doctor may suggest you have more frequent exams.
DIALATED EYE EXAMS
Early detection and treatment can prevent vision loss. If you are diabetic, be sure to schedule a comprehensive dilated eye exam at least twice a year. It is important to remember that your diabetic retinopathy can progress without symptoms. You can develop both proliferative retinopathy and macular edema and still see normally, but you may remain at high risk for vision loss. A retina specialist can tell if you have any stage of diabetic retinopathy or macular edema. Depending on the severity of your diabetic retinopathy, your doctor may suggest you have more frequent exams.
BLOOD SUGAR CONTROL
Better control of blood sugar levels slows the onset and progression of retinopathy. In general, diabetic patients who kept their blood sugar levels as close to normal as possible also had significantly less kidney and nerve disease. Better control also reduced the need for sight-saving treatment. Patients should routinely see their primary care provider who can determine the best form of blood sugar control for you. Control of associated Hypertension and blood cholesterol is also advised for optimal result.
EARLY SYMPTOMS
There are often no symptoms during the early stages of the disease, nor is there any pain. It's important, therefore, not to wait for symptoms. When symptoms do occur, they range from mildly blurred central vision to complete vision loss. It specifically causes problems in reading and near vision. It is critical to secure prompt medical attention if you notice any change in your vision.
SYMPTOMS OF ADVANCED DISEASE
Proliferative retinopathy frequently produces symptoms as a result of bleeding into the vitreous cavity. At first, you may notice a few specks of blood "floating" in your vision. If that occurs, see your retina specialist as soon as possible; you may need treatment before more serious bleeding occurs. Hemorrhages tend to happen more than once, often during sleep. Sometimes, even without treatment, the spots clear, and your vision will improve. Yet it's more likely that bleeding will reoccur and cause severely blurred vision. You need to be examined by your retina specialist at the first sign of blurred vision, before more bleeding occurs. The earlier you receive treatment, the more likely treatment will be effective. If left untreated, proliferative retinopathy can cause severe vision loss and even blindness.
Diabetic retinopathy is detected during a comprehensive eye exam. After checking your vision and eye pressure, drops are placed in your eyes to widen, or dilate, the pupils. A retina specialist uses a special magnifying lens to examine your retina for signs of diabetic retinopathy.
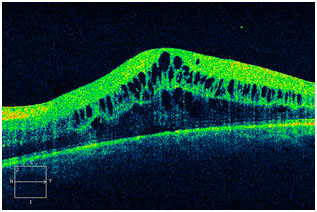
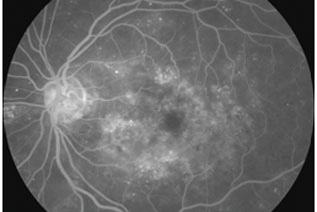
Your retina specialist may also order special testing to help stage the retinopathy or decide if treatment is needed. One test, a fluorescein angiogram, uses a special dye that is injected into your arm. Pictures are taken as the dye passes through the blood vessels in your retina, allowing for the identification of any leaking blood vessels that may require treatment. Your doctor may also recommend Ocular Coherence Tomography, or OCT, to check for diabetic macular edema. This is a non-invasive test, similar to an ultrasound or CT scan, that helps detect fluid within the macula. After the exam, your close-up vision may remain blurred for several hours due to the dilating drops.
During the stages of mild and moderate non-proliferative diabetic retinopathy, no treatment is needed unless macula edema is present. To prevent the progression of diabetic retinopathy, people with diabetes should control their blood sugar, blood pressure and cholesterol.
FOCAL/ GRID LASER TREATMENT
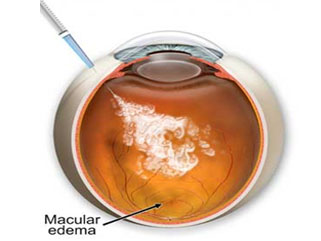
Macular edema is most effectively treated with focal laser treatment that is usually completed in one session. Your doctor seals leaking blood vessels (microaneurysms) with light heat generated by a laser. These treatment spots slow the leakage of fluid and reduce the amount of fluid in the macula. Focal laser treatment slows the rate of vision loss by about 50 percent and can improve visual acuity. You may need focal laser more than once to control the leaking fluid. For more wide-spread macular swelling (edema), grid laser is often used.
Both focal and grid laser treatments are performed in your doctor's office with the lights dimmed. Before the treatment, your physician will dilate your pupil and apply drops to numb the eye. As you sit facing the laser machine, your doctor will hold a special lens to your eye. During the procedure, you will see flashes of bright light. Although the flashing lights are often described as annoying, there is generally little to no discomfort associated with this procedure.
Laser treatment will at best stabilize vision, but generally cannot restore vision that has been lost. This is yet another reason that treating diabetic retinopathy early is the best way to prevent vision loss.
INTRAVITREAL INJECTIONS
Certain drugs have been used to successfully reduce macular edema and new blood growth resulting from diabetic retinopathy
Anti-VEGF Injection Therapy. Anti-VEGF drugs are injected into the vitreous gel to block a protein called vascular endothelial growth factor (VEGF), which can stimulate abnormal blood vessels to grow and leak fluid. Blocking VEGF can reverse abnormal blood vessel growth and decrease fluid in the retina. Available anti-VEGF drugs include Avastin (bevacizumab), Lucentis (ranibizumab), and Eylea (aflibercept). Lucentis and Eylea are approved by the U.S. Food and Drug Administration (FDA) for treating DME. Avastin was approved by the FDA to treat cancer, but is commonly used to treat eye conditions, including DME.
Most people require monthly anti-VEGF injections for the first 3-6 months of treatment. Thereafter, injections are needed less often.
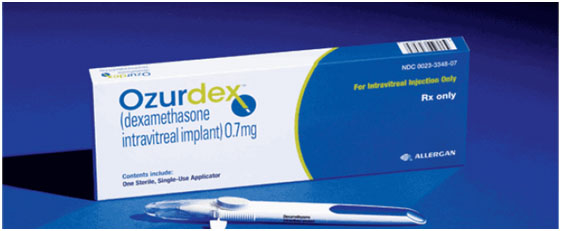
Corticosteroids. Corticosteroids, either injected or implanted into the eye, may be used alone or in combination with other drugs or laser surgery to treat DME. The Ozurdex (dexamethasone) implant is for 6 months duration, while Triamcinolone (tricort) is for 2 months duration. Corticosteroid use in the eye increases the risk of cataract and glaucoma (much more with tricort than Ozurdex).
There are two major therapies for proliferative diabetic retinopathy—Pan retinal photocoagulation laser treatment and vitrectomy.
PANRETINAL PHOTOCOAGULATION
Scatter laser treatment helps to shrink the abnormal blood vessels. Your doctor places laser spots throughout the entire peripheral retina, causing the abnormal blood vessels to shrink. Because it's necessary to use a large number of laser spots, more than one session (3-4) is often required to complete treatment. Scatter laser treatment is needed to preserve your central vision. This treatment is more effective before the fragile, new blood vessels have started to bleed, even if bleeding has begun, scatter laser treatment may still be possible, based on the amount of bleeding

In some instances, anti-VEGF drugs may be used in conjunction with laser to treat severe forms of proliferative diabetic retinopathy.
Some degree of discomfort is common with this treatment. It usually subsides at the end of the procedure, but some patients report mild discomfort or a mild headache lasting for the rest of the day. Other complications are rare, but will be explained prior to your procedure.
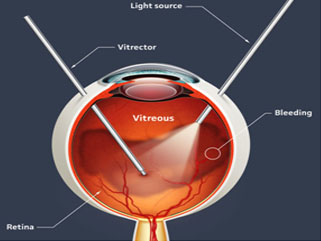
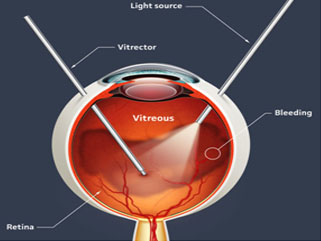
VITRECTOMY

You may require a surgical procedure called a vitrectomy if bleeding is severe, if it does not clear up on its own or if you develop a retinal detachment related to your diabetic retinopathy. This procedure is almost always performed under local anesthesia. Your doctor inserts tiny instruments through small incisions in the sclera (the white portion of the eye) and removes the gel and blood from the center of the eyeball. He or she will then replace the clouded gel with a clear saline solution or gas bubble or silicone oil. Following the procedure, an eye patch is placed on the operated eye and you need to return to the office the next day.
Both are very effective in reducing vision loss. Although they both have high success rates, neither one cures diabetic retinopathy, but rather reduces the risk of new bleeding. Vitrectomy surgery can—and usually does—improve vision, but scatter laser is employed to stabilize vision. You may need multiple treatments to protect your sight.
Ask your retina specialist about referring you to a low vision specialist and about low vision services and devices that may help you make the most of your remaining vision.
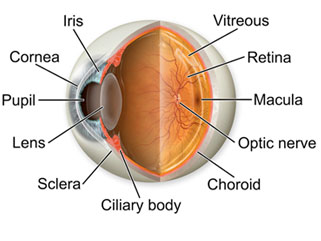
Glaucoma is a disease of the optic nerve. The optic nerve is a connection between the eyeball and the brain which transmits the images you see from the eye to the brain. The optic nerve is made up of many nerve fibers (like an electric cable with its numerous wires).
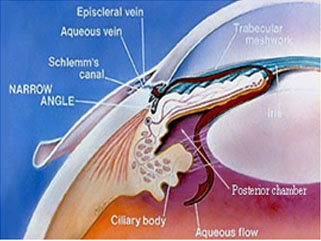
Glaucoma damages nerve fibers, which can cause blind spots and vision loss. Glaucoma has to do with the pressure inside the eye, known as intraocular pressure(IOP) . The aqueous humor (a clear liquid that normally flows in and out of the eye) is normally produced in the eye and it drains out of the eye via small drainage system known as Trabecular meshwork. When the aqueous humor cannot drain properly, pressure builds up in the eye. The resulting increase in IOP can damage the optic nerve and lead to vision loss.
When intraocular pressure (IOP) is above normal range (10 – 22 mm Hg) the risk of developing glaucoma increases.
There are mainly two types of glaucoma
Open angle glaucoma: Most people who develop primary open-angle glaucoma notice no symptoms with vision being normal initially but in late stages when their vision is impaired. It starts from decrease in peripheral vision and then involves central vision in the end.
Angle closure glaucoma: It is an emergency with symptoms of headache, nausea, vomiting, coloured haloes and sudden decrease in vision.
1. Increased IOP
2. Age > 40 years
3. Family history of glaucoma
4. Ethnic background like African American, Asians, Hispanics
5. Diabetes, heart conditions, blood pressure, hypothyroidism, migraine
6. History of injury to eye, long term use of steroids ( especially in allergies), high myopia (minus numbers)
1. Tonometry: checking your IOP in a painless manner.
2. Vision testing and Visual field testing on Perimeter
3. Gonioscopy: a special contact lens is put on the eye after instilling anaesthetic drops to evaluate the drainage system of the eye
4. Slit lamp biomicroscopy: to check the status of your optic nerve
5. Optical coherence tomography (OCT): it is the most definitive and advanced test to check the status of your optic nerve and to monitor progression and decide treatment protocol.
The goal of glaucoma treatment is to lower your intraocular pressure. Glaucoma can't be cured, and damage caused by the disease can't be reversed, but treatment and regular check-ups can prevent vision loss in people with early glaucoma. If vision loss has already occurred, treatment can slow or prevent further vision loss.
Open angle glaucoma: Treatment is in form of eye drops and oral medications in order to decrease production of aqueous humor in the eye or improve drainage or both. Do remember to discuss with your doctor about the dosage and possible side effects of the medication
In scenario where treatment is ineffective or there is intolerance to medication other options are:
1. Laser therapy: laser trabeculoplasty as an OPD procedure may be performed to improve the aqueous humor drainage. It is performed after anesthetising the eye with topical anaesthetic drops and placing a special contact lens on the eye and firing laser shots to open up the trabecular meshwork.
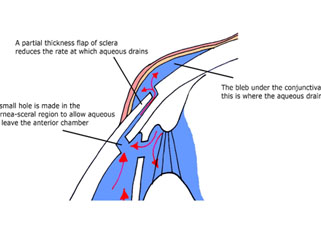
2. Filtering surgery: It is known as trabeculectomy. It is performed as an in-patient procedure in the operation theatre. Here local anaesthesia is given and a small piece of the drainage system is removed to bypass the block and create an alternative pathway for the aqueous humor drainage. Discuss the success ratio and the possible complications and the after care of the surgery with your doctor.
This needs urgent treatment to reduce the pressure in your eye. This generally will require both medication and procedures.
Oral medications and eye drops are given in the initial phase to reduce the eye pressure and decreasing the pain of the patient. Later stage requires a procedure called laser peripheral iridotomy (LPI).
In LPI doctors create a small hole in your iris using a laser so that fluid (aqueous humor) can flow through it and exit your eye. Doctors will evaluate your other eye and may recommend an iridotomy in it, because of the high risk that its drainage angle also will close in the future.
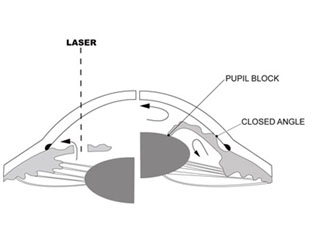
Many patients are found during screening to be at risk of angle closure glaucoma in which case the doctor will advise to undergo prophylactic LPI to prevent future complications.
What can you do to prevent blindness from glaucoma?
Proper compliance to prescribed medication and regular check-up is a must. All patient with the above said risk factors should get screened for glaucoma
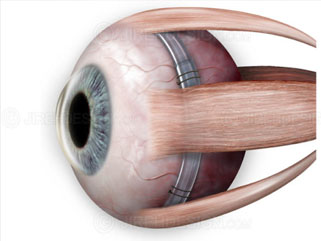
Uveitis is the inflammation of the uvea, the middle layer of your eye. The eye is shaped much like a ball, with three different layers of tissue surrounding a central gel-filled cavity. The inner most layer is the retina, which senses light and helps to send images to you brain. The middle layer between the sclera and the retina is called the uvea. The outer most layer is called the sclera, the strong white wall of the eye which is for protecting the eye.
The uvea contains many blood vessels, the veins and the arteries that carry blood flow to the eye. Since it nourishes many important parts of the eye (such as the retina), inflammation of the uvea can damage your site. The Eye receives the maximum supply of blood in the body after the brain.
What are the symptoms of the uveitis?
Symptoms of uveitis include:
Uveitis may come on suddenly with the redness and pain, or sometimes with painless blurring of your vision. It can be a potential blinding of the eye if left untreated.

A case of simple "red eye" may in fact be serious problem of the uveitis. If your eye becomes red or painful, and does not clear up quickly, you should be examined and treated by an ophthalmologist. Hence never ignore a red eye with reduction in vision as it may be a harbinger sight threatening disease.
Uveitis has many different causes:
In most cases of uveitis, the cause remains unknown. Almost 80% of the cases no cause may be found inspite of undergoing a battery of investigation.
How is uveitis diagnosed?
A careful eye examination by an ophthalmologist is extremely important when symptoms occur. Inflammation inside the eye can permanently effect sight or even lead to blindness, if it is not treated. A therough slit lamp and a dialeted fundus exam is mandatory in every case.
Your ophthalmologist will examine the inside of your eye. Many times Oct scan (for the detailed imaging of the retinal layers) and FFA (fundus angiography) is done for further understanding of the disease
He or she may order blood tests, skin tests or X-rays to help make the diagnosis.
Since uveitis can be associated with disease in the rest of the body, your ophthalmologist will want to know about your overall health. He or she may want to consult with your physician or other medical specialists.
Are there different kinds of uveitis?
There are different types of uveitis, depending on which part of the eye is affected:

Uveitis can lead to cystoid macular edema ( accumulation of fluid in the retinal layers)
Uveitis is a serious eye condition that may scar the eye leading to permenant visual handicap hence you need to have it treated as soon as possible.
Eye drops, especially steroids and pupil dilators, can reduce inflammation and pain. For more severe inflammation, oral medication or injections may be necessary. Oral steroids and antimetabolities may also be used in very serious cases.
Many times steroid injections in form of Triamcinolone or Dexamethasone implants (Ozurdex) are given intravitreally (inside the eye) for curing the cystoid macular edema and vitreous inflammation
Uveitis can have these complications:
These complications may also need treatment with eye drops, conventional surgery or laser surgery. If you have a "red eye" that does not clear up please see your ophthalmologist urgently
Occlusion (blockage) of a retinal vein is a common cause of sudden painless reduction in vision in older people.
The retina is the thin membrane that lines the inner surface of the back of your eye. Its function is similar to that of the film in a camera. Blockage of one of the veins draining blood out of the eye causes blood and other fluids to leak into the retina, causing bruising and swelling as well as lack of oxygen. This interferes with the light receptor cells (cells responsible for vision) and reduces vision.
The condition is uncommon under the age of 60 but becomes more frequent in later life.
There are two types of retinal vein occlusion
It causes painless loss of vision, In general, visual loss is more severe if the central retinal vein is blocked.

A blockage forms in the vein, usually due to a blood clot, and obstructs the blood flow. The exact cause is unknown, but several risk factorsmake the condition more likely. These include
The complications of RVO, especially if they are not treated, can lead to irreversible loss of vision
Since there is no cure for either BRVO or CRVO, the focus of management is on the following:
The evaluation and treatment of underlying risk factors (e.g., diabetes or hypertension), leading to improved treatment of systemic problems and prevention of heart attack and stroke.
The evaluation and treatment of complications such as macular edema and neovascularization, leading to preservation of vision.
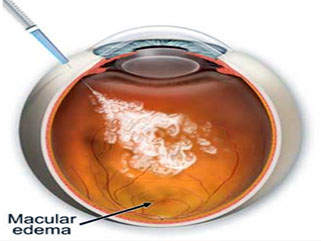
MACULAR EDEMA
Two medications currently being used, Lucentis® / Accentrix (ranibizumab) and Avastin® (bevacizumab), have both been successful in reducing the edema and improving vision in both BRVO and CRVO. A third medication, Eylea® (aflibercept), is effective for treating edema secondary to RVO.
A common treatment approach is to start with 2-3 monthly injections and continue as needed over the next several months.
Complications are rare, but can include a) infection (endophthalmitis) b) retinal detachment and c) vitreous hemorrhage, all of which are related to the injection itself and not specifically to the medications.
Although only Lucentis and Eylea are approved by the FDA for treatment, Avastin is also commonly used in this manner, and all are thought to be effective and equally safe for the eye.
Steroids: Steroids are another type of medication that can decrease macular edema. Similar to Lucentis, Eylea and Avastin, the steroid is injected directly into the vitreous through the sclera. Two of the most commonly used steroids are preservative-free Triamcinolone Acetonide Suspension and Ozurdex (a dexamethasone implant). The primary difference between them is that the effect of Ozurdex is longer in the eye than triamcinolone (6 months versus 2 months). The complication of steroid induced glaucoma and cataract progression is much more with thriamcinolone than Ozurdex.
Repeat injection are required frequently over the course of the disease.
NEOVASCULARIZATION
Laser photocoagulation: Laser is the best way to control and decrease neovascularization in either BRVO or CRVO. A stronger laser is applied to the affected region of the retina. Mild peripheral vision loss can sometimes occur.
Vitreous hemorrhage and tractional retinal detachment:If the retina specialist is unable to perform the laser treatment due to either a vitreous hemorrhage or retinal detachment, a vitrectomy will be recommended. A vitrectomy is an outpatient surgical procedure performed in an operating room that involves removal of the vitreous from the inside back of the eye through three openings made in the sclera using a microscope and several small instruments. Now a days Micro incision sutureless vitrectomy (MIVS) is done using 25 and 27 Gauge instruments
Neovascular glaucoma
Treatment includes control of Intraocular pressure (IOP) via topical, oral and systemic medications. Also it is required to treat the underlying retinal disease which is causing tremendous amounts of VEGF via PRP laser, AntiVEGF injections and Cryopexy. In some cases antiglaucoma surgery in form of Trabeculectomy with MMC or Valve surgery is required.
As with any treatment, it is critical that patients have a thorough discussion with their retina specialist regarding all of the treatment options, including the risks, benefits and alternatives, before deciding the appropriate course of action.
Cystoid macular edema is a painless disorder which affects the central retina or macula. When this condition is present, multiple cyst-like (cystoid) areas of fluid appear in the macula and cause retinal swelling or edema.
Symptoms
Blurred or decreased central vision. If you experience this symptom, contact your eye doctor for a complete exam.

Causes
Although the exact cause of CME is not known, it may accompany a variety of diseases such as retinal vein occlusion, uveitis, or diabetes. It most commonly occurs after cataract surgery.
Risk Factors
About
1-3 % of those who have cataract extractions will experience decreased vision due to CME, usually within a few weeks after surgery. If the disorder appears in one eye, there is an increased risk (possibly as high as 50%) that it will also affect the second eye. Fortunately, however, most patients recover their vision with observation or treatment.
How is cystoid macular edema diagnosed?
Cystoid macular edema is usually diagnosed three ways:
Anti-VEGF agents – Ranibizumab (Accentrix), and Bevacizumab (Avastin) act by decreasing vascular permeability from disrupted endothelial cells.
Some cases do require repeat injections for permanent cure.
Surgery - Sometimes, the vitreous (the gel that fills most of the back of the eye) pulls on the macula causing CME (vitreomacular traction).
The retina is the light-sensitive layer of tissue that lines the inside of the eye and sends visual messages through the optic nerve to the brain. There is a jelly called vitreous which is present in the eye attached to the retina and supporting the retina. In case when the vitreous undergoes change to a liquid it separates from the retina, this is perceived as floaters or black dots in front of the eye.
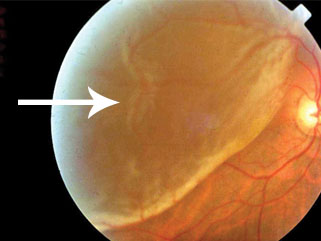
In some cases there may be small areas of the retina that are torn when the vitreous has separated from the retina and pulled the retina. These areas, called retinal tears or retinal breaks or retinal holes, can lead to retinal detachment due to fluid of the eye leaking through this opening
When the retina detaches, it is lifted or pulled from its normal position. If not promptly treated, retinal detachment can cause permanent vision loss.
There are three different types of retinal detachment:
A retinal detachment can occur at any age, but is more likely to occur in people who:
Symptoms include a sudden or gradual increase in either the number of floaters, which are little "cobwebs" or specks that float about in your field of vision, and/or light flashes in the eye. Another symptom is the appearance of a curtain over the field of vision. A retinal detachment is a medical emergency. Anyone experiencing the symptoms of a retinal detachment should see an eye care professional immediately.
Small holes and tears are treated with laser or by a freeze treatment called cryopexy. These procedures are usually performed in the doctor's office. Laser is used to surround the break and seal it and / or "weld" the retina back into place. Cryopexy freezes the area around the hole and helps reattach the retina.
Retinal detachments are treated with surgery that may require the patient to stay in the hospital. In some cases a scleral buckle, a tiny synthetic band, is attached to the outside of the eyeball to gently push the wall of the eye against the detached retina. If necessary, a vitrectomy may also be performed. During a vitrectomy, the doctor makes a tiny incision in the sclera (white of the eye). A small instrument is used to remove the vitreous. Silicon oil is injected in the eye to replace the vitreous and support the retina. Silicon oil is removed at alter date at the doctors decision. Sometimes Gas is used to support and reattach the retina. During the healing process, the eye makes fluid that gradually replaces the gas.
Prognosis
With modern therapy, over 90 percent of those with a retinal detachment can be successfully treated, although sometimes a second treatment is needed. However, the visual outcome is not always predictable. The final visual result may not be known for up to several months following surgery. Even under the best of circumstances, and even after multiple attempts at repair, treatment sometimes fails and vision may eventually be lost.
Visual results are best if the retinal detachment is repaired before the macula (the center region of the retina responsible for fine, detailed vision) detaches. That is why it is important to contact an eye care professional immediately if you see a sudden or gradual increase in the number of floaters and/or light flashes, or a dark curtain over the field of vision.
Prevention
Use protective eye wear to prevent eye trauma. Control your blood sugar carefully if you have diabetes. See your eye care specialist twice a year. You may need more frequent visits if you have risk factors for retinal detachment. Be alert to symptoms of new flashes of light and/or floaters.
ALWAYS GET YOUR EYES CHECKED TWICE A YEAR